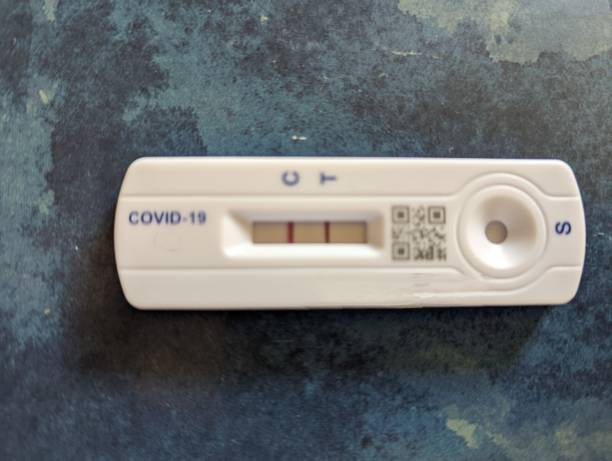
An antigen test is easier since it just needs smaller, portable instruments, while molecular rapid antigen tests need specialist equipment for processing samples. Their structure resembles, let’s say, a pregnancy test.
How is the exam conducted? Antigen assays look for SARS-CoV-2 viral protein fragments. A healthcare practitioner uses a reagent to prepare the sample you provide before doing an immediate analysis. These rapid antigen tests, in contrast to molecular testing, need a larger concentration of virus in the test sample in order to be positive. Thus, a false negative result from an antigen test is sometimes possible.
How exactly is a sample taken? In order to collect a specimen, much as with molecular testing, a sterile swab is put into your nose or throat (see details above), however, throat swabs could be less usual these days.
How are test results handled?
A test strip or cartridge is self-applied with the sample. Results are shown as a colored line to indicate positive or negative, much like a home pregnancy test.
Where may one be purchased?
At addition to being available in pharmacies and medical offices, rapid antigen tests may also be bought for use at home.
How soon can you provide results?
Typically, results are available in 10 to 15 minutes.
Just how precise are they? Antigen test sensitivity varies with the stage of an infection, according to the CDC, but is regarded as having “moderate to high” sensitivity at peak viral load. Antigen testing is more prone than molecular rapid antigen tests to provide false negative findings, particularly when conducted on individuals who don’t exhibit symptoms. You can also read about Rapid antigen tests that come to be done at home by visiting http://corewellnesspdx.com/rapid-antigen-tests-that-come-be-done-at-home/
What about rapid antigen tests taken at home?
All of the rapid antigen tests use antigen. However, there are home molecular science kits that call for shipping a sample to a lab. The cost of a home test, which may range from $24 for a set of two to $38 for one, may not be paid by your insurance company, in contrast to testing at pharmacies and physicians’ offices, which is often free or covered by insurance.
If you want a fast response, Dr. Campbell advises using home testing. The problematic issue, he adds, is that costs may add up and that test-takers don’t always answer questions truthfully. It’s crucial to properly follow the instructions.
The FDA advises serial testing—or taking numerous rapid antigen tests—over a number of days to increase the likelihood of finding asymptomatic illnesses since they are less sensitive than a molecular test.
However, Dr. Campbell suggests utilizing testing carefully in light of the present test scarcity.

“I would hold off on doing a home antigen test until around three days following a confirmed COVID exposure if you have access to one. If the results are bad, I’ll try again on days five and seven,” he adds. “Even those are many rapid antigen tests. Therefore, depending on the extent of your exposure and whether you develop symptoms, you may not need to continue testing, particularly if you are immunized and considered to be at “low risk.” Test once again when your symptoms have subsided and you are prepared to resume work.
According to Dr. Campbell, the fundamental rule of testing in the medical field is to conduct an experiment only when the outcome would alter your course of action. According to him, if you are exposed to COVID and subsequently have symptoms, there is a good possibility that you are infected given the current high incidence rate levels. If you can safely treat your symptoms at home and you can isolate them, you should do so.
Dr. Campbell also advises keeping in mind that if an antigen test is positive right now, it is most likely correct.
“Those who now have a positive antigen test are virtually probably contagious and infectious. At worst, those who are antigen-negative are less infectious. Because the studies are difficult to do, we can’t declare with certainty that they are not communicable, but they are undoubtedly less contagious,” he adds. “False positives begin to outweigh genuine positives when the incidence of illness is very low. False positives, however, are quite improbable right now because of the high prevalence.
What kind of test should I go for?
Health professionals suggest that regardless of whether you have had a vaccine, you should be checked if you have a fever, cough, breathing difficulties, or other COVID-19 symptoms. Dr. Campbell continues, “If testing is available, think about testing three to five days following a high-risk exposure.”
Making the choice of test type might be difficult.
“Access and what is easily accessible to you determine a lot of this. Although we are grateful for fast antigen testing, their sensitivity is limited if you don’t have symptoms, and 40% of COVID carriers are asymptomatic, according to Dr. Martinello. “A NAAT test is more sensitive, but the quality of the material still matters a lot,”
However, clinicians will often utilize a PCR test to diagnose very unwell patients (with a suspected case of COVID-19), since false-negative testing might lead to insufficient therapy. You can also read about Getting a PCR test to check if you have coronavirus (COVID-19) by clicking here.
Travel You may also need to be tested if you’re traveling. It’s possible that the place you’re going calls for certain testing procedures and authorized testing sites.
“In my opinion, the exam you may take is the most appropriate for travel at the moment. Great if you can get PCR. If not, get an antigen, advises Dr. Campbell. However, you should test since you don’t want to be the one who spreads the illness to the rest of the passengers.
Both workplaces and schools
For how they provide COVID-19 testing, schools may have their own set of guidelines. Antigen testing, however, is effective for monitoring in areas like schools and workplaces, according to Dr. Campbell.
Say you, test students, twice a week for the rest of the time at a school. If you employ antigen testing, you may do it considerably more quickly, conveniently, and affordably, according to him. “You need to determine whether or not children are contagious right now. Would PCR be more effective there? Yes, but you won’t always receive a response right away, and it would cost a lot of money to locate a few successes. Speed is sometimes the most crucial factor.
Peace of mind
For peace of mind, some persons may like to have regular COVID exams. Consider a scenario in which you are immunized yet want to visit an old relative or attend a crowded event.
You should test beforehand to ensure you aren’t the one transmitting a virus if you’re planning to do something unsafe and then visit your 90-year-old mother, he advises.

The timing of what to do next is challenging
“If you attended a crowded concert and are concerned about COVID, you shouldn’t take any COVID rapid antigen tests the following day, whether they be molecular or rapid antigen tests. After a probable exposure, you should wait three to five days, advises Dr. Campbell. We believe that a sufficient quantity of virus must be present for a person to be contagious, and we are aware that the viral load fluctuates during an illness.
Dr. Campbell says that if you just have a few tests available, you should use them shortly before visiting susceptible friends or family members—or right before attending an event with thousands of people. He advises using them to prevent the spread of disease.